Introduction:
Enhanced DNA damage repair effect is an important mechanism for drug-resistance in chronic lymphocytic leukemia (CLL). Moreover, the ability of cancer cells to repair under radiation or chemotherapy drug induced DNA damage also serves as one of the mechanisms for therapy resistance. It is reported that nucleolar and spindle associated protein 1 (NUSAP1), a microtubule binding protein, has been involved in DNA damage repair process and plays important roles in the development, progression, and metastasis in several types of cancer. However, its role and mechanism in the development of CLL are still unclear.
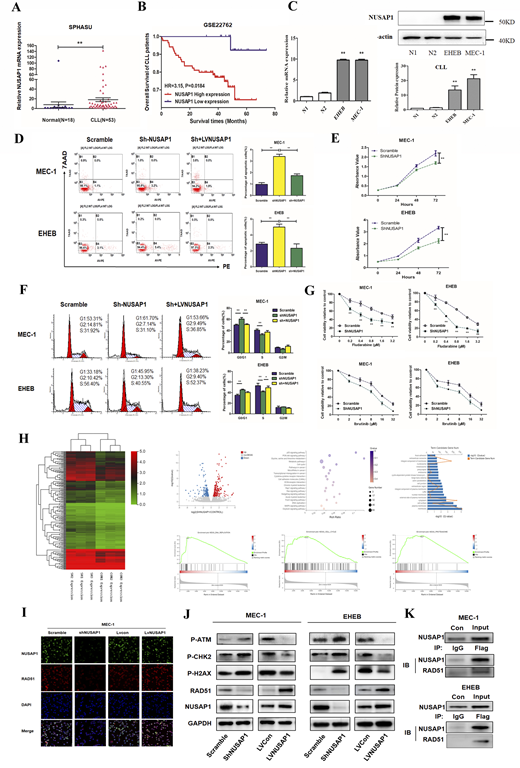
Methods: Expression levels of NUSAP1 mRNA and protein in CLL cell lines and patient specimens were detected by qRT-PCR and Western blot, and Kaplan-Meier survival curve and overall survival were analyzed by log-rank test. Peripheral blood samples from de novo CLL patients and healthy volunteers were collected with informed consents at the Department of Hematology in Shandong Provincial Hospital Affiliated to Shandong University (SPHASU). Microarray datasets GSE22762 were obtained from Gene Expression Omnibus. With altering NUSAP1 expression by lentivirus-transfected cells in vitro, the effects of NUSAP1 on cell proliferation, apoptosis and cycle were detected by CCK8, Annexin V-PE /7AAD staining and PI/RNase staining respectively. Bioinformatics analysis, luciferase reporter analysis, immunoprecipitation and were applied to discern and examine the relationship between NUSAP1 and its potential targets.
Results: According to clinical specimens and bioinformatics analysis, the expression level of NUSAP1 gene in samples of CLL patients was significantly increased than that of healthy donors (P<0.05) (Figure A). Besides, the results indicated that the OS of patients with highly expressed NUSAP1 was significantly worse than in patients with low expression with the statistical analysis database GSE22762. mRNA and protein expression levels of NUSAP1 were significantly higher in CLL cell lines than in PBMCs from healthy donors (Figure C). Our findings indicated that NUSAP1 knockdown notably inhibited cell proliferation when compared with the Scramble group (Figure D). Moreover, the amounts of DNA fragmentation of the apoptotic cells were remarkably increased by NUSAP1 shRNA in MEC-1 and EHEB cells when compared with the Scramble group (Figure E). In addition, after knocking down NUSAP1, MEC-1 and EHEB cells were blocked in G0/G1 phase (Figure F). Moreover, addition to fludarabine or ibrutinib with shNUSAP1 group showed enhanced cytotoxicity in CLL cells (Figure G). The differential genes were analyzed via RNA-seq between Scramble and ShNUSAP1 group. Intriguingly, annotations of gene ontology (GO) analysis indicated that NUSAP1 was closely related to biological processes including cell cycle and response to drug. Kyoto encyclopedia of genes and genomes (KEGG) analysis showed that NUSAP1 were enriched in pathways in cancer, DNA replication and cell cycle. Gene set enrichment analysis (GSEA) implicated that NUSAP1 was functionally enriched in DNA replication, cell cycle and proteasome (Figure H). Immunofluorescence showed that NUSAP1 was mainly distributed in the cell nucleus, and the expression level of RAD51 was positively correlated with the change of NUSAP1 expression (Figure I). Surppression of NUSAP1 inhibited the action of proteins in DNA damage repair pathway (Figure J). Through COIP, NUSAP1 was identified to bind with RAD51 and play an important role in DNA damage repair pathway (Figure K). Hence, NUSAP1 participates in the DNA damage repair process and enhances the drug resistance in CLL.
Conclusions: This study first demonstrated that the high expression of NUSAP1 in CLL patients is associated with poor prognosis through database analysis and experiments in vitro. Interference of NUSAP1 expression led to a slower CLL cell proliferation and a higher apoptosis rate, meanwhile induced the G1 phase arrest. Collectively, our findings demonstrated that NUSAP1 contributes to DNA damage repairing by binding to RAD51 and enhances drug resistance in CLL. Therefore, NUSAP1 is expected to be a potential target for the treatment of CLL with drug-resistance.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal